We Wish to Inform You That Your Pap Smear Came Back Abnormal
Most women who receive abnormal cervical cancer screening results either have human papillomavirus (HPV) infections or have early cell changes that can be monitored (since they often go away on their own) or treated early (to prevent the development of cervical cancer). The information on this page can help you to learn more about abnormal cervical cancer screening results and follow-up tests and treatments.
HPV Infection
Human papillomaviruses (HPVs) are a group of related viruses, some of which are spread through sexual contact. Some of these HPV types, called high-risk HPV, cause nearly all cases of cervical cancer. They can also cause anal cancer, penile cancer, vaginal cancer, vulvar cancer, and oropharyngeal cancer (cancer in the throat, usually the tonsils or the back of the tongue).
Learn more about how HPV causes cancer in HPV and Cancer.
HPV Test and Pap Test (Pap Smear)
The HPV test and the Pap test are two different cervical cancer screening tests. Screening means checking for a disease or for changes that may develop into disease before there are symptoms. Women need routine cervical cancer screenings even if they feel fine. Screening can help find changes in cervical cells so you can receive the proper follow-up care and treatment you need to stay healthy.
The HPV test checks cells for infection with high-risk HPV types.
The Pap test (also called a Pap smear or cervical cytology) collects cervical cells and looks at them for changes caused by HPV that may—if left untreated—turn into cervical cancer. It can also detect cervical cancer cells. A Pap test also sometimes finds conditions that are not cancer, such as infection or inflammation.
The HPV/Pap cotest uses a Pap test and HPV test together to check for both high-risk HPV and cervical cell changes.
What to Expect during an HPV or Pap Test
The cervix is part of the female reproductive system. It's the lower, narrow end of the uterus, which leads to the vagina, as shown in the image above. The cervix opens during childbirth to allow the baby to pass.
Both types of cervical cancer screening tests are usually done during a pelvic exam, which takes only a few minutes. During this exam, you lie on your back on an exam table, bend your knees, and put your feet into supports at the end of the table. The health care provider uses a speculum to gently open your vagina in order to see the cervix. A soft, narrow brush or tiny spatula is used to collect a small sample of cells from your cervix.
The sample of cervical cells is sent to a lab, where the cells can be checked to see if they are infected with the types of HPV that cause cancer (HPV test). The same sample can be checked for abnormal cells (Pap test/Pap smear). When both an HPV test and a Pap test are done on the same sample, this is called HPV/Pap cotesting.
A pelvic exam may include more than taking samples for an HPV and/or Pap test. Your health care provider may also check the size, shape, and position of the uterus and ovaries and feel for any lumps or cysts. The rectum may also be checked for lumps or abnormal areas. Most health care providers will tell you what to expect at each step of the exam, so you will be at ease. You may also ask to be tested for sexually transmitted infections (STIs), also called sexually transmitted diseases (STDs).
Where to Get Cervical Cancer Screening: Clinics that Offer Screening
Doctors' offices, clinics, and community health centers offer HPV and Pap tests. Many women receive these tests from their ob/gyn (obstetrics/gynecology) or primary care provider. If you don't have a primary care provider or doctor you see regularly, you can find a clinic near you that offers cervical cancer screening by contacting:
- your state or local health department
- the National Breast and Cervical Cancer Early Detection Program (NBCCEDP) or call 1-800-232-4636; NBCCEDP provides low-income, uninsured, and underserved women access to timely cervical cancer screening and diagnostic services
- a Planned Parenthood clinic, or call 1-800-230-7526
- NCI's Cancer Information Service (CIS), or call 1-800-422-6237
Questions to Ask Before and After Your Exam
Before Your Exam:
Ask your health care provider:
- What tests will I have?
- What is the purpose of these tests?
- What will happen during the exam?
- Will I have any discomfort?
Your health care provider may ask you:
- What was the start date of your last menstrual period?
- When did you have your last cervical cancer screening test?
- Have you ever had any abnormal test results or treatment for abnormal cells on your cervix?
After Your Exam:
Ask your health care provider:
- When will I get my test results?
- How will I get these results (e.g., by mail, online, or a phone call)?
- What phone number should I call if I do not get my test results?
- When I get my results, will they explain what I should do next?
Screening Guidelines: When and How Often to Get Screened for Cervical Cancer
Cervical screening recommendations have been developed by several organizations, including the United States Preventive Services Task Force (USPSTF), the American Cancer Society (ACS), and others.
The details of the recommendations vary, but all are based on research findings, including:
- HPV-caused changes in cervical cells happen slowly and often go away on their own, especially in younger women
- more effective screening tests
- the harms of overtesting and overtreatment for cervical changes that would have gone away on their own
Age 21–29 years: USPSTF recommends that women get their first Pap test at age 21 and have Pap testing every 3 years. Even if a woman is already sexually active, Pap tests are not recommended until the age of 21.
Age 30–65 years: USPSTF recommends that women in this age group be screened for cervical cancer using one of these methods:
- HPV test every 5 years
- HPV/Pap cotest every 5 years
- Pap test every 3 years
ACS has recently published updated cervical cancer screening guidelines that recommend women start screening at age 25 with an HPV test and have HPV testing every 5 years through age 65. However, testing with an HPV/Pap cotest every 5 years or a Pap test every 3 years is still acceptable. To read about the reasons for the changes, see ACS's Updated Cervical Cancer Screening Guidelines Explained.
Older than 65 years: Women in this age group should talk with their health care provider to learn if screening is still needed. If you have been screened regularly and had normal test results, your health care provider will probably advise you that you no longer need screening. However, if your recent test results were abnormal or you have not been screened regularly, you need to continue screening beyond age 65.
Exceptions to the Guidelines
Your health care provider may recommend more frequent screening if you:
- are HIV positive
- have a weakened immune system
- were exposed before birth to a medicine called diethylstilbestrol, (DES) which was prescribed to some pregnant women through the mid 1970s
- had a recent abnormal cervical screening test or biopsy result
- have had cervical cancer
Women who've had an operation to remove both their uterus and cervix (called a total hysterectomy) for reasons not related to cancer or abnormal cervical cells do not need to be screened for cervical cancer. However, if your hysterectomy was related to cervical cancer or precancer, talk with your health care provider to learn what follow-up care you need. Women who've had an operation to remove their uterus but not their cervix (sometimes called a partial or supracervical hysterectomy) should continue routine cervical cancer screening.
HPV Test Results: What a Positive or Negative Result Means
HPV test results show if high-risk HPV types were found in cervical cells. An HPV test will come back as a positive test result or a negative test result:
- Negative HPV test result: High-risk HPV was not found. You should have the test again in 5 years. You may need to come back sooner if you had abnormal results in the past.
- Positive HPV test result: High-risk HPV was found. Based on your specific test result, your health care provider will recommend follow-up steps you need to take.
HPV test results usually come back from the lab in about 1–3 weeks. If you don't hear from your health care provider, call and ask for your test results. Make sure you understand any follow-up visits or tests you may need.
What does it mean if a woman has a positive HPV test after years of negative tests?
Sometimes, after several negative HPV tests, a woman may have a positive HPV test result. If you have a new sexual partner, this is most likely a new infection. If you do not have a sexual partner, or if you are in a monogamous relationship, this is not necessarily a sign of a new HPV infection, and it doesn't mean that your partner has a new sexual partner. Sometimes an HPV infection can become active again after many years. Some other viruses behave this way as well; for example, the virus that causes chickenpox can reactivate later in life to cause shingles.
There is no way to tell whether a newly positive HPV test result is a sign of a new infection or a reactivation of an old infection. Researchers don't know whether a reactivated HPV infection has the same risk of causing cervical cell changes or cervical cancer as a new HPV infection.
Pap Test Results: What a Normal, Abnormal, or Unsatisfactory Result Means
Pap test results show if cervical cells are normal or abnormal. A Pap test may also come back as unsatisfactory.
- Normal Pap test results: A normal test result may also be called a negative test result or negative for intraepithelial lesion or malignancy. If only the Pap test was done, you should have the next test in 3 years. If the Pap test was done together with an HPV test (this is called a Pap/HPV cotest), you can have the next test in 5 years. You may need to come back sooner if you had abnormal results in the past.
- Abnormal Pap test results: An abnormal test result may also be called a positive test result. An abnormal test result does not mean you have cervical cancer. Possible abnormal findings on a Pap test include ASC-US, AGC, LSIL, ASC-H, HSIL, AIS, or cervical cancer. Your health care provider will recommend follow-up steps you need to take based on your specific test result and your past test results.
- Unsatisfactory Pap test results: The lab sample may not have had enough cells, or the cells may have been clumped together or hidden by blood or mucus. Your health care provider will usually ask you to come in for another screening test in 2 to 4 months.
Pap test results usually come back from the lab in about 1-3 weeks. If you don't hear from your health care provider, call and ask for your test results. Make sure you receive your test results and understand any follow-up visits or treatments that you need.
- Atypical Squamous Cells of Undetermined Significance (ASC-US) is the most common abnormal Pap test finding. It means that some cells don't look completely normal, but it's not clear if the changes are caused by HPV infection. Other things can cause cells to look abnormal, including irritation, some infections (such as a yeast infection), growths (such as polyps in the uterus), and changes in hormones that occur during pregnancy or menopause. Although these things may make cervical cells look abnormal, they are not related to cancer. Your health care provider will usually do an HPV test to see if the changes may be caused by an HPV infection. If the HPV test is negative, estrogen cream may be prescribed to see if the cell changes are caused by low hormone levels. If the HPV test is positive, you may need additional follow-up tests.
- Atypical Glandular Cells (AGC) means that some glandular cells were found that do not look normal. This can be a sign of a more serious problem up inside the uterus, so your health care provider will likely ask you to come back for a colposcopy.
- Low-Grade Squamous Intraepithelial Lesions (LSIL) means that there are low-grade changes that are usually caused by an HPV infection. Your health care provider will likely ask you to come back for additional testing to make sure that there are not more serious (high-grade) changes.
- Atypical Squamous Cells, cannot exclude HSIL (ASC-H) means that some abnormal squamous cells were found that may be a high-grade squamous intraepithelial lesion (HSIL), although it's not certain. Your health care provider will likely ask you to come back for a colposcopy.
- High-Grade Squamous Intraepithelial Lesions (HSIL) means that there are moderately or severely abnormal cervical cells that could become cancer in the future if not treated. Your health care provider will likely ask you to come back for a colposcopy.
- Adenocarcinoma in situ (AIS) means that an advanced lesion (area of abnormal growth) was found in the glandular tissue of the cervix. AIS lesions may be referred to as precancer and may become cancer (cervical adenocarcinoma) if not treated. Your health care provider will likely ask you to come back for a colposcopy.
- Cervical cancer cells (squamous cell carcinoma or adenocarcinoma) are sometimes found on a Pap test. However, this finding is very rare for women who have been screened at regular intervals. You can learn more about cervical cancer, including staging and treatment options, in Cervical Cancer Treatment (PDQ ®).
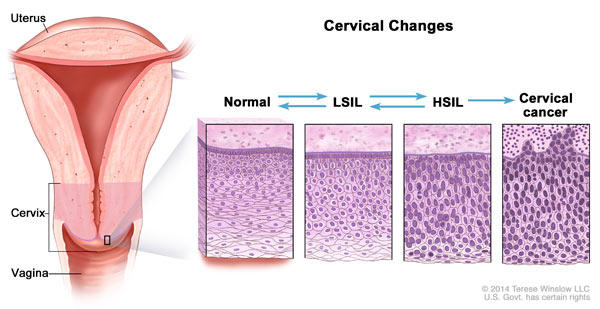
These images show how cervical cells that have long-lasting infections with high-risk HPV can change over time and become abnormal. Abnormal cervical cells may also return to normal even without treatment, especially in younger women. LSIL and HSIL are two types of abnormal changes to cervical squamous cells.
Follow-up Tests and Procedures after an Abnormal Pap or HPV Test
Keep in mind that most women with abnormal cervical screening test results do not have cancer. However, if you have an abnormal test result, it's important to get the follow-up care that your health care provider recommends.
Next Steps after an Abnormal Pap Test, HPV Test, or HPV/Pap Cotest
Until recently, follow-up recommendations were based on the results of a woman's most recent screening test. However, updated ASCCP risk-based management consensus guidelines advise a more tailored approach to follow-up care.
What these updated guidelines mean is that, in addition to your current Pap, HPV, or cotest screening result, your health care provider will consider additional factors when recommending follow-up care, including:
- previous screening test results,
- previous treatments for precancerous cervical cell changes, and
- personal health factors, such as your age.
Based on your individual risk of developing severe cervical cell changes that could become cervical cancer, you may be advised to:
- return for a repeat HPV test or HPV/Pap cotest in 1 or 3 years
- have a colposcopy and biopsy
- receive treatment; see Treatment for High-Grade Cervical Cell Changes
These updated guidelines focus on detecting and treating severe cervical cell changes that could develop into cervical cancer while also decreasing testing and treatment for less severe conditions (low-grade cervical cell changes).
Colposcopy and Cervical Biopsy
Colposcopy and biopsy are two procedures that allow a closer look at the cells of your cervix.
During a colposcopy your health care provider inserts a speculum to gently open the vagina and view the cervix. A vinegar solution will be applied to the cervix to help show abnormal areas. Your health care provider then places an instrument called a colposcope close to the vagina. It has a bright light and a magnifying lens and allows your health care provider to look closely at your cervix.
A colposcopy usually includes a biopsy. A small piece of cervical tissue will be removed, or a procedure called endocervical curettage will be used to take a sample of abnormal tissue from the cervix. These cervical cells are then checked under a microscope for signs of disease.
Talk with your health care provider to learn what to expect during and after your biopsy procedure. Some women have bleeding and/or discharge after a biopsy. Others have pain that feels like cramps during menstruation.
Biopsy Findings: Cervical Intraepithelial Neoplasia (CIN)
Biopsy samples are checked by a pathologist for cervical intraepithelial neoplasia (CIN). CIN is the term used to describe abnormal cervical cells that were found on the surface of the cervix after a biopsy.
CIN is graded on a scale of 1 to 3, based on how abnormal the cells look under a microscope and how much of the cervical tissue is affected. LSIL changes seen on a Pap test are generally CIN 1. HSIL changes seen on a Pap test can be CIN 2, CIN2/3, or CIN 3.
- CIN 1 changes are mild, or low grade. They usually go away on their own and do not require treatment.
- CIN 2 changes are moderate and are typically treated by removing the abnormal cells. However, CIN 2 can sometimes go away on its own. Some women, after consulting with their health care provider, may decide to have a colposcopy with biopsy every 6 months. CIN 2 must be treated if it progresses to CIN 3 or does not go away in 1 to 2 years.
- CIN 3 should be treated right away, unless you are pregnant.
Treatment for High-Grade Cervical Cell Changes
These treatments are used when a woman has high-grade cervical cell changes that have a high risk of developing into cancer.
Treatments that remove abnormal cells are called excisional treatments:
- Cold knife conization: A scalpel is used to remove a cone-shaped section of abnormal tissue. This procedure is done at the hospital and requires general anesthesia.
- LEEP (loop electrosurgical excision procedure): A thin wire loop, through which an electrical current is passed, is used to remove abnormal tissue. Local anesthesia is used to numb the area. Your health care provider usually performs this procedure in the office. It takes only a few minutes, and you will be awake during the procedure.
Treatments that destroy abnormal cells are called ablative treatments:
- Cryotherapy: A special cold probe is used to destroy abnormal tissue by freezing it. This procedure is done in your health care provider's office. It takes only a few minutes and usually does not require anesthesia.
- Laser therapy: A laser (narrow beam of intense light) is used to destroy abnormal tissue. This procedure is done at the hospital and general anesthesia is used.
Pregnancy and Treatment for High-Grade Cervical Cell Changes
If you are pregnant or plan to become pregnant, your health care provider will talk with you about procedures that are recommended for you and the timing of these procedures. Depending on your specific diagnosis, you may be treated postpartum, or after delivery.
Questions to Ask Before Treatment
- What are the possible treatments for the condition that I have?
- Which treatment do you recommend for me, and why?
- What are the advantages and disadvantages of this treatment?
- What will happen during the treatment?
- What are the possible risks of this treatment?
- How might this treatment affect a future pregnancy?
- How long will the procedure take?
- Will general anesthesia or local anesthesia be needed?
- What side effects might I have from this procedure? How long might these side effects last?
- Are there any activities that I should avoid after the procedure?
We Wish to Inform You That Your Pap Smear Came Back Abnormal
Source: https://www.cancer.gov/types/cervical/understanding-abnormal-hpv-and-pap-test-results
Post a Comment for "We Wish to Inform You That Your Pap Smear Came Back Abnormal"